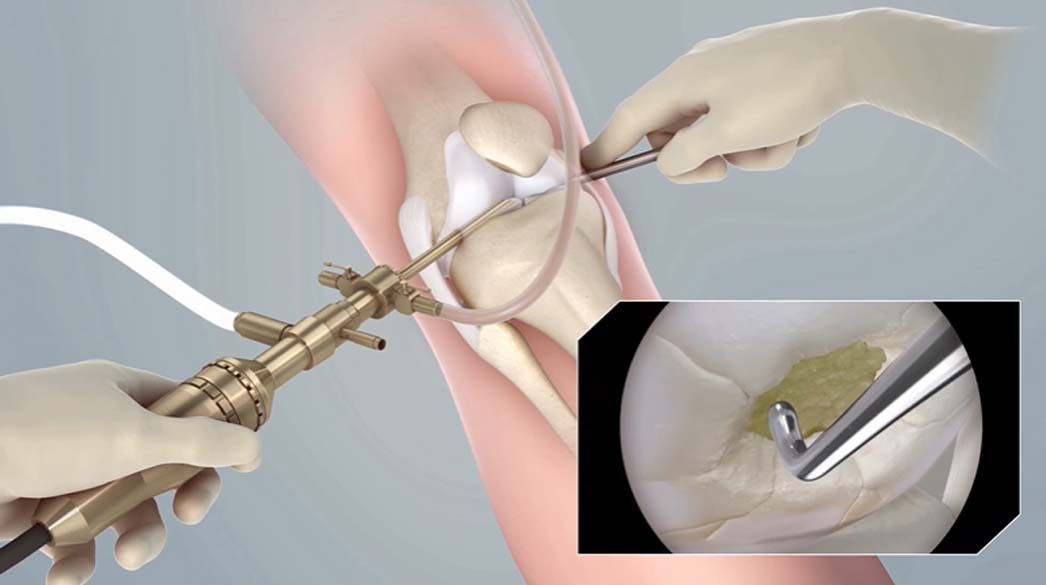
The first surgical step in pursuing the MACI procedure for articular cartilage repair requires an arthroscopy. An arthroscopy is a minimally invasive procedure that allows a physician to scope the knee, diagnose the causes of knee pain and perform other surgical repairs. The arthroscopy is phase one in MACI knee cartilage repair. It allows the surgeon to take a cartilage biopsy of a patient's own cells, which is later used to grow new cartilage tissue and implant it into the patient's knee. During an arthroscopy, a physician may also remove loose fragments of bone or cartilage and repair damaged ligaments or meniscus.
MACI® (autologous cultured chondrocytes on porcine collagen membrane) is made up of your own (autologous) cells that are expanded and placed onto a film that is implanted into the area of the cartilage damage and absorbed back into your own tissue. MACI is used for the repair of symptomatic cartilage damage of the adult knee. It is not known whether MACI is effective in joints other than the knee. It is not known whether MACI is safe or effective in patients over the age of 55 years.
What to Expect During an Arthroscopy
An arthroscopy is generally conducted on an outpatient basis, meaning the procedure does not require an overnight hospital stay. During the arthroscopy, a physician sedates a patient using one or a combination of the anesthesia options below.
- Local anesthesia. This form of anesthesia is injected into the knee joint to numb the area. The patient will be awake for the procedure and may feel some pressure but no pain.
- Regional anesthesia. The patient will receive an injection to the lower back or leg. This form of anesthesia will numb the area below the patient's waist. With regional anesthesia, the patient will be awake during the procedure but will feel no pain.
- General anesthesia. For longer arthroscopies, physicians may recommend the patient receive general anesthesia. This type of anesthesia is delivered intravenously and puts the patient in a sleep-like, pain-free state.
Once the patient is sedated, the surgeon will make a few small incisions (each about a buttonhole size) into the knee. The physician will insert a tiny tube attached to a fiber-optic camera into one of these portals to inspect the joint. The other incisions will be used for surgical tools to perform repairs or gather biopsies. The surgeon may inject a sterile solution into the knee that expands the area around the joint to provide a better view.
Next, the surgeon diagnoses the knee and conducts the necessary surgical procedures. When performing an arthroscopy on MACI eligible patients, the physician will determine the size, location and bone involvement of the patient's knee cartilage damage — and take two to three cartilage samples from non-weight bearing areas of the knee for use in MACI knee cartilage regeneration.
The procedure is generally brief, about 30 minutes to one hour. Upon completion, the incisions will be closed with one to two stitches each or adhesive tape. Following the procedure, the patient will recover in a separate room. After a few hours, when the patient can stand and walk from a bed to a chair, the patient will be released to go home.
What to Expect After an Arthroscopy
Every patient is unique. Often, patients report their knee cartilage pain temporarily improves after an arthroscopy, given the surgeon's efforts to remove damaged knee structures and make minor repairs. While this procedure can provide some relief, it will not repair cartilage defects, and symptoms may return.
Given cartilage defects don't heal on their own and can worsen over time, physicians may recommend patients pursue additional treatment for knee cartilage pain after an arthroscopy to provide long-lasting relief and improve quality of life.
In the case of a patient who chooses MACI, the cartilage biopsy gathered during an arthroscopy is sent to our FDA-licensed facilities, where the cells are embedded in a cartilage membrane, treated and multiplied to grow a new cartilage implant from the patient's own cells. It will take approximately one month of processing before the new cartilage tissue is ready to be implanted in a patient's knee during a second follow-up procedure. This cartilage implant will be stored in a cryopreservation tank at our facilities for several years to allow the patient and surgeon to schedule a procedure when it's most convenient.
Please see below for full indication and ISI. Blog posts are intended to provide educational information. Always talk to your doctor with any questions.